Reflecting on “medical assistance in dying” or MAID
Since June 2016, 15 months into the newly changed law, over 2,000 Canadians who applied for “medical assistance in dying” have died by procedures that previously were referred to as assisted suicide or euthanasia. Where does it leave those who believe that life as a gift of God is sacred? As Bishop Colli reminded us in his June 2016 letter, “medically assisted death is unacceptable and morally wrong according to the standards of our Catholic teaching”. Are Catholics then expected to suffer through the final stage of their life, waiting for a natural death while others can avail themselves of a medical intervention that will lead to a swift death? Does this moral prohibition create a terrible burden on Catholics? I will suggest that this is not the case. True, there is a price for being a disciple in the form of work and effort required, but there are also vital, tangible benefits.
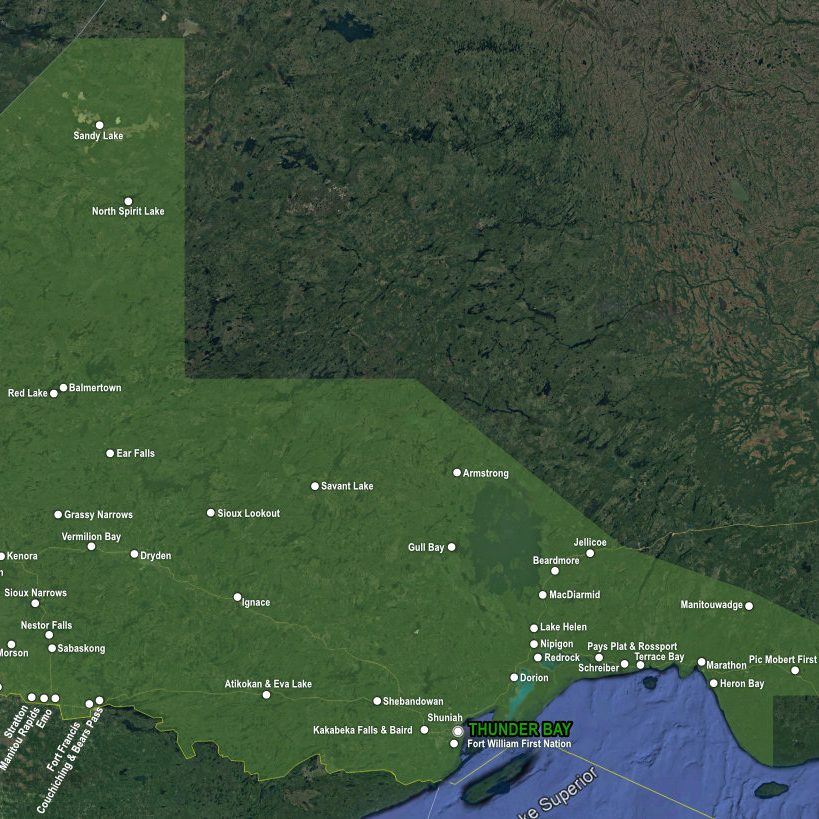
Let us say that someone close to you is thinking about having their life terminated by a medical practitioner. If you are concerned that this is morally wrong or problematic and you want to be helpful, then at the least, try to make sure that the person has taken these two important steps. The first step is to ask the doctor for a palliative care consultation. The second step is to seek a person who would be an attentive’ listener’ and guide for the person who is near death. The goal of palliative care is to make possible the best quality of life for people with incurable conditions by relieving troublesome symptoms and sources of suffering, without aiming either to prolong the life or shorten it. Many family doctors are good in controlling suffering caused by pain, nausea, shortness of breath, constipation and other symptoms, but if problems persist, it is good to know that doctors and nurses who are specialists in palliative care are masters in this field of pain control. In our city and region, we have excellent palliative care professionals. If requested, the family doctor or home care nurse will arrange for a visit and follow up with a palliative care professional for the patient. Palliative medication that is taken with the intent to control pain, but may unintentionally shorten one’s life is morally permissible and is not considered either assisted suicide or euthanasia.
It can often be the case that a patient whose pain and physical suffering has been brought under control may still feel miserable. He or she may see themselves as a burden on the family or society, feel hopeless and useless, experience anxiety and fear further deterioration or death. Even a Catholic, who fervently believes in life after death, may feel that life has lost its meaning and can despair when death is near. During this time of emotional, existential and spiritual anxiety, the patient may greatly benefit from, what I call here, the second step, that is, from sharing his or her thoughts and feelings with an individual who can really ‘listen’ and guide them through their suffering. A good ‘listener’ will encourage the sick to talk about what concerns them while maintaining confidentiality; will ensure them that they will not be judged for what they disclose; and guide them to understand that they are valued and good, if for no other reason than they are loved unconditionally by God. This valuable aid can be given by a parish priest, a minister, a deacon, a pastoral care person, a spiritual director, a counsellor, a social worker, a trained palliative care volunteer, a wise family member or friend. Through active listening and counseling, the patient may be helped to recall the blessings received,recognize how he or she has been a blessing to others, and may see their past life in a new and positive light. Then, even their relationship with God will be strengthened. The patient may need help to realize that their remaining life, however short it will be, can have a deep and serious meaning and is precious. Indeed, there may be some important goals that the dying person and only that person can achieve, such as to forgive past injustices and receive forgiveness from others, reconcile sons and daughters who have been estranged, give wise guidance to the spouse and children for their future life, or simply have time to express their love and gratitude.
After these two steps, more can be done, and that is to accompany the person, day by day, as he or she approaches natural death. A person who decides to be such a companion may find this role very challenging, and may find that asking for support of extended family and friends and various organizations is necessary in order to persevere in this role. But what could be seen as a burden can be transformed into a commitment of love and sacrifice of one’s time and energies, as long as the companion accepts one’s limitations and allows God to work in one’s life. What we propose is not always effective or acceptable to the suffering person. Yet, with proper medical care and the support of a community of love, a person approaching death may come to realize that medical assistance in dying is not the solution to their agonizing feelings, and that the natural, unplanned dying process may actually be a culmination of their life and bring a new dynamism to the whole family. Many great things can happen around the bed of the dying, especially when pain is controlled and the dying person is valued, validated and affirmed. Some suffering may persist but it can become bearable and have personal meaning if the patient can join his or her suffering with that of Christ and is supported by loved ones.
It must be noted that some people, even with the best possible care and effective comfort measures, will remain determined to obtain medically assisted death if they meet the conditions of the law. We have to recognize that they have a legal right to seek assisted death and we cannot put obstacles in their way. Then, perhaps the only thing one can do is to pray. The expression “Death with Dignity” has lately been attached to medically induced dying in order to boost the appeal of such acts. Yet, what has a better claim for death with dignity? A quick, medicalized death delivered by an impersonal, technical procedure or a deliberate thoughtful, unhurried affair, a surge of love that is a real culmination of the life well lived? A true death with dignity is possible to achieve when the dying person knows that God, one’s family, friends and meaningful individuals love them unconditionally, accept them for what they are, and ultimately support them as they prepare to die a natural death.
Jaro Kotalik, MD
Comments or questions? Please contact jkotalik@tbaytel.net
The entire “Reflecting on Medical Assistance in Dying” Maid Document is available via pdf.